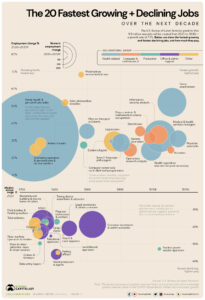
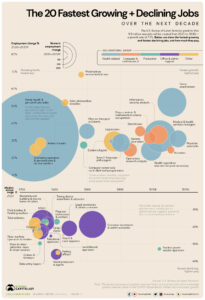
On 13 September 2021, visualcapitalist.com published ‘The 20 Fastest Growing Jobs in the Next Decade’ written by Jenna Ross:
“How is the Job Market Shifting Over the Next Decade?
The employment landscape is constantly shifting. While agricultural jobs played a big role in the 19th century, a large portion of U.S. jobs today are in administration, sales, or transportation. So how can job seekers identify the fastest growing jobs of the future?
The U.S. Bureau of Labor Statistics (BLS) projects there will be 11.9 million new jobs created from 2020 to 2030, an overall growth rate of 7.7%. However, some jobs have a growth rate that far exceeds this level. In this graphic, we use BLS data to show the fastest growing jobs.
We used the dataset that excludes occupations with above average cyclical recovery from the COVID-19 pandemic. For example, jobs such as motion picture projectionists, ticket takers, and restaurant cooks were removed. Once these exclusions were made, the resulting list reflects long-term structural growth.
Here are the fastest growing jobs from 2020 to 2030, along with the number of jobs that will be created and the median pay for the position.
| Occupation |
Percent employment change, 2020–2030P |
Numeric employment change, 2020-2030P |
Median annual wage, 2020 |
| Wind turbine service technicians |
68.2% |
4,700 |
$56,230 |
| Nurse practitioners |
52.2% |
114,900 |
$111,680 |
| Solar photovoltaic installers |
52.1% |
6,100 |
$46,470 |
| Statisticians |
35.4% |
14,900 |
$92,270 |
| Physical therapist assistants |
35.4% |
33,200 |
$59,770 |
| Information security analysts |
33.3% |
47,100 |
$103,590 |
| Home health and personal care aides |
32.6% |
1,129,900 |
$27,080 |
| Medical and health services managers |
32.5% |
139,600 |
$104,280 |
| Data scientists and mathematical science occupations, all other |
31.4% |
19,800 |
$98,230 |
| Physician assistants |
31.0% |
40,100 |
$115,390 |
Nine of the top 20 fastest growing jobs are in healthcare or related fields, as the baby boomer population ages and chronic conditions are on the rise. Home health and personal care aides, who assist with routine healthcare tasks such as bathing and feeding, will account for over one million new jobs in the next decade. This will be almost 10% of all new jobs created between 2020 and 2030. Unfortunately, these workers are the lowest paid on the list.”
We ask ourselves, how does this picture unfold in South Africa, and the answer is similar to the article written by Jenna Ross.
According to logicpublishers.com : Jobs That Will Be In Demand In The Next 5-10 Years In South Africa (4May 2021)
“Since technology and the rest of the world are advancing rapidly, it can be hard to know how the labour market will look like in the next five to ten years. Fortunately, according to the current progress, specific jobs with growth potential have become supreme contenders.
- Software Developer
A software developer is one of the fastest-growing jobs with best outlook. Unless you have been lying under a rock for the last 20 years, you already know the vast roles these professionals play in everyday life.
- Medical And Health Service Manager
A medical and health service manager role is one of the most-demanding jobs in the next 5-10 years. The healthcare industry is extensive and complicated and providing care for patients is only part of the job. A medical service manager’s role is to collect payments, schedule appointments, keep medical records and coordinate with other care providers.
- Post-secondary Teacher
A post-secondary teacher is one of the best careers for the future as people seek advanced education from every part of the world. College professors provide the final transitional resources between young adults and the real world. Students attend college to earn practical skills in their profession hence the importance of a post-secondary teacher. One of the most amazing things about this career choice is that it is something that one is passionate about. It is flexible and pays well.
- Nurse Practitioner
A nursing practitioner is a registered nurse with advanced training in primary care services. This way, they can perform certain functions ordinarily done by doctors, such as ordering medication, lab test and x-rays. Considering the importance of health, a nurse practitioner is one of the most-demanded professions, which will likely grow.
- Financial Manager
If you are looking for a career that will give you excellent financial stability, then one as a financial manager is one of the best. Remember that every firm, regardless of its size, requires someone to handle the money. And big business procures the services of a financial manager that is among the best-paying high-demand jobs in the next 5-10 years. Financial managers create reports and assist in directing the organization’s long-term financial goals.
- Solar Photovoltaic Installers
As the world is going green, people are looking for renewable and sustainable energy solutions, and solar panels are one of the most popular. This has resulted in great demand for solar photovoltaic installers that promises a good salary. These professionals install solar panel systems according to the client’s needs and specifications.
- Wind Turbine Technicians
With a post-secondary non-degree award and sufficient on-the-job training, you can become a professional wind turbine technician. The profession is amongst the best career for the next ten years as people are going for renewable energy. Wind turbine installers install and maintain renewable energy systems.
- Personal Care Aides
Personal care aides are one of the most influential people in the health care profession. They serve the population requiring extra assistance with their daily living requirements. However, people in this profession concentrate more on non-medical services. Regular duties include meal planning, preparation, dressing, bathing, housekeeping duties and many more.
- Statisticians
A statistician is one of the fastest growing jobs with a bachelor’s degree. What does a statistician do? They analyze and apply data in a wide array of fields. Since they hold advanced knowledge in statistical interpretation, they are an integral piece of government research institutions and other firms.
- Physical Therapist Assistants
A physical therapist’s aide role is to assist the physical therapist with the patient’s appointment and set up equipment for upcoming meetings, among numerous other functions. The responsibilities also vary by the area of practice. One can secure a job in residential care facilities, private physical therapy offices or via government services.
- Bicycle Repairers
In recent years, people have discovered the importance of bicycle riding to their health and are adopting the culture. The prevalence of the practice has contributed to the rising demand for bicycle repairers. Ordinarily, bicycle repair technicians assess and solve maintenance issues of bicycles regardless of their complexity. Such professionals find employment in bike shops, sporting goods stores, non-profit organizations and other areas.
- Occupational Therapy Assistants
Have you ever thought of a career in occupational therapy? It is one of the best careers for the next ten years, considering the growing demand for occupational therapy. As the name suggests, an occupational therapy assistant aids the therapist with specific duties like stretching, rehabilitative exercises and many more.
- Informational Security Analyst
An informational security analyst is one of the most promising careers to pursue, considering the direction the world is taking. The development of technology and its adoption in various aspects of people’s lives has created a significant risk that information system analysts must review. A big part of this job is protecting computer networks and systems from cybercrime. Therefore, these professionals will install antivirus software and other safeguards to protect information.
- Accountants And Auditors
Whatever business you are in, you require your financial records to be in good order. One needs to learn if their business is making a profit or loss. That is where accountants come in – they help manage a business’s accounts, including taxes.
- Management Analysts (a.k.a. Consultants)
Managers always seek solutions to problems, and it is the analyst’s role, popularly known as the consultant, to make this happen. It is one of the best jobs with growth potential and with an excellent annual income. A management analyst is required to provide revenue increasing and cost-cutting solutions to make a firm more profitable. The profession pays pretty well, but it requires frequent travelling.
- Construction Managers
Construction managers are responsible for erecting new structures that are cropping up everywhere in a business-oriented environment. A construction manager is in charge of a construction project and ought to make all the operational decisions.
- Dental Hygienist
Dentists are integral in oral healthcare, and it is one of the most demanding jobs in the next 10 years. Everyone requires dental services at some point in their lives, so it is a demanding job.
- Civil Engineers
Civil engineers are vital to a country’s growth and citizen’s well-being. They are responsible for ascertaining that people have access to clean water in numerous circumstances like after a hurricane.
- Computer System Analyst
As the name suggests, a computer system analyst is responsible for all the computer-related activities in a firm. Firms usually have more than one computer systems analyst with different roles and a manager overseeing their operation. This is one of the most promising careers since all significant firms have computer systems.”

Shire is proud to be part of Project Scaffold.
Project Scaffold has been developed as a voluntary pilot programme that will gather and test results from ten participating frail care facilities to pave the way towards a new dispensation. The main objective is to develop a home-like environment that is person-centred and more affordable. We, like many countries abroad, believe that hospital-like care needs to make way for person-focused care. Project Scaffold, although not a crisis management tool, hopes to facilitate the sharing of best practices within the sector throughout the duration of the project.
A Care Transformation Toolkit (CTT) has been compiled for the use of those care centres selected to participate in Project Scaffold.
Support is available on request from the following participants:
1. Syd Eckley (Consult Age), a gerontologist and social worker who will mainly be responsible for assessing compliance in terms of Act 13/06.
2. Rob Jones (Shire), an experienced consultant on retirement living and associated services, including care.
3. Magda Pienaar & Yolandé Brand (true2you), specialising in facilitating the creation and/or implementation of person-directed care and organisational cultures.
To read more about Project Scaffold, click here.